Insulin Detection of Clinical Plasma Samples
Development of a PDMS microfluidic system.
By Zhikun Zhan, Zaili Dong, and Steve Tung
NOTE: This is an introduction to the article, which appeared in the September 2011 issue of the IEEE Nanotechnology magazine.
Click here to read the article.
Diabetes mellitus is a group of diverse metabolic disorders caused by deficiency or diminished effectiveness of endogenous insulin. It is the third leading cause of disease-related death around the world after cancer and cardiovascular disease. At present, the blood glucose test is the most popular clinical diagnostic tool for diabetes, but irregular blood glucose level, unfortunately, is not a good early indicator for diabetes diagnosis. Previous studies have shown that insulin, connecting peptide, and interleukin-6 are better suited as early diagnostic immune indicators for the onset of diabetes.
Insulin, a hormone produced by the pancreas for converting glucose to energy, is a common clinical indicator. Its abnormity can be detected as an effective auspice to diagnose diabetes at an early stage, which is helpful for diabetes prevention. The traditional test methods for insulin and other indicators in clinical diagnosis, which include enzyme-linked immunosorbent assay (ELISA), radioimmunoassay, and various chemiluminescence-based techniques, are usually based on microplates and large automatic biochemistry analyzers. These methods, while effective, are predominantly laboratory based and require trained technicians. This makes them unsuitable for field testing, which is becoming increasingly important for diabetes screening in developing countries.
The article describes a PolyDiMethySiloxane (PDMS)-based microfluidic system with pneumatic micropumps and micromixers has been developed for high-accuracy insulin detection of clinical plasma samples. The detection method is based on double-antibody sandwich immunoassay coupled with luminol-hydrogen peroxide (H2O2) chemiluminescence.
Microfluidics, with advantages such as low reagent consumption, short analysis time, high reliability and sensitivity, and multiprocess integration, is a rapidly developing field in biomedical testing. In microfluidic systems, the conventional biochemical processes, such as sample pretreatment, sample/reagent transport, mixing, reaction, separation, detection, and product collection, can be carried out automatically on a single chip [6]. Additionally, microfluidic systems have become the most promising tool for handling costly and difficult-to-obtain samples and reagents. More importantly, the portability characteristic of these systems that arises from their compact form is a key factor for point-of-care applications and offers a practical solution to diabetes screening in a rural environment.
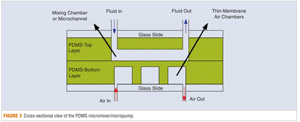
The article describes in some detail the materials, chemical methods, and composition of the microfluidic system. Figure 3 from the article shows a view of one of the micromixer/micropump assemblies used.
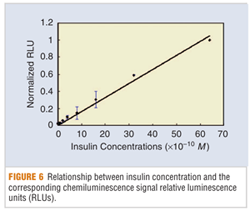
Tests were performed on the microfluidic device to analyze serum samples from diabetic patients. The results of those tests are given in the article. Figure 6 from the article shows the detected signal from the device as a function of the insulin concentration.
The authors conclude that their study demonstrates the application of a PDMS microfluidic system for insulin detection of clinical plasma samples based on heterogeneous chemiluminescent immunoassays. The detection method utilizes two pneumatic micropumps operated at a flow rate of about 10µL/min and a micromixer operated at a frequency of 5 Hz. The detection limit of the PDMS microfluidic system is 10-11M with a linear range of 5 X 10-10 M to 6.4 X 10-9M. The detection time is about 10 min., which is more than ten times faster than that of the conventional methods for insulin detection.
AUTHORS
Zhikun Zhan (Zhanzhikun2010@gmail.com) was a Ph.D. student at the State Key Laboratory of Robotics, Shenyang Institute of Automation, Chinese Academy of Science, when the research work described in the article was carried out. Currently, she is a lecturer at the Automation Department, Institute of Electrical Engineering, Yanshan University, China.
Zaili Dong (dzl@sia.cn) is a professor at the State Key Laboratory of Robotics, Shenyang Institute of Automation, Chinese Academy of Science.
Steve Tung (chstung@uark.edu) is an associate professor at the Department of Mechanical Engineering at the University of Arkansas.