A View From the Outside In
By Leslie Mertz
NOTE: This is an abstract of the entire article, which appeared in the September/October 2011 issue of the IEEE Pulse magazine.
Click here to view the entire article.
In today’s operating rooms, surgeons are more likely to be scrutinizing a computer screen than examining a patient’s opened chest or abdominal cavity. In just a few short years, imaging techniques such as computed tomography (CT), magnetic resonance (MR) tomography, and ultrasound have graduated from tools that help a doctor diagnose a health condition to tools that can actually guide therapy. Doctors are currently using these imaging techniques to navigate the brain during neurosurgery, to perform virtual colonoscopies, and to pinpoint the location and size of malignant tumors to help ensure their complete removal. This is just the beginning, according to experts in the field.
Research is under way to expand the use of image-guided therapies so that surgeons can perform heart-valve replacements and other cardiovascular procedures without having to cut the chest cavity. Additional studies are ongoing to use image-guided therapy for pancreatic and other cancers that are now difficult or nearly impossible to treat and for the development of new drug delivery systems that will transport chemotherapeutic agents to the target site, and only to the target site, thereby drastically reducing a patient’s drug dose and the associated side effects.
Dieter Haemmerich, Ph.D., associate professor of pediatrics at the Medical University of South Carolina. He described the main imaging technologies:
- CT, which uses X-rays to obtain data that are constructed into cross-sectional or other images
- MR imaging (MRI), which uses a magnetic field and radio waves to produce images
- ultrasound imaging, which uses ultrasonic waves to create representations of internal body structures.
The entire article describes a number of areas where image-guided therapy is making valuable inroads into patient treatment.
The primary job of image-guided therapy is to provide a useful and detailed picture of the inside of the body. In cancer treatment, it means finding a tumor and determining its exact boundaries. Robert L. Galloway, Jr., Ph.D., professor of biomedical engineering, professor of surgery, professor of neurosurgery, and director of the Center for Technology Guided Therapy at Vanderbilt University, describes the “registration” problem – how a scanned image relates to physical space. The single leading step in image-guided therapy is therefore this registration between image space and physical space. He said. “We try to provide that information in such a way that the surgeon can construct the 3-D image in his or her head and determine the relative positions of the structures in the patient.”
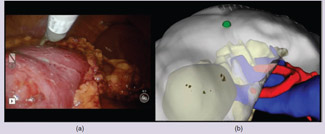
Image guidance in neurosurgery is now the standard of care, and may become the expected approach in other medical procedures. Dr. Galloway points out that image guidance would also be important in abdominal surgery, where organs are heavily vascularized – with the associated danger of cutting major blood vessels. The article presents advances in image-guided systems in liver, kidney, and pancreatic surgery (Figure 1).
Figure 1 (a) The traditional laparoscopic view of the kidney when using the da Vinci Surgical System (Intuitive Surgical Inc., Sunnyvale, CA). (Photo courtesy of Dr. Robert Galloway and Rowena Ong.)
(b) Work done at Vanderbilt University adds image guidance to the system via the operating room image-oriented navigation (ORION) system and allows the surgeon to see structures beneath the surgical tool as they operate.
Image-guided technologies are finding a place in heat-ablation procedures that turn up the temperature on tumors until their cells die. Haemmerich is conducting research on the use of electric current to heat tissues, a procedure known as radio frequency (RF) ablation, which is already in use clinically. “In this case, a catheter is run through a small incision in the skin, and inserted into the tumor using image guidance. Then, the tumor and the surrounding tissue are heated and destroyed by heat. The heat is used to directly kill the cancer.” It is not always 100% successful, he said. “One limitation is still that sometimes you kill most of the tumor but not all of it, and then the tumor grows back. This research is to try to get better heating devices to uniformly kill the whole tumor.”
“Nonlethal heat and radiation is also a winning combination, because the heat makes the tumor cells more susceptible to radiation”, said Neal Kassell, M.D., professor of neurosurgery at the University of Virginia and chair of the Focused Ultrasound Surgery Foundation. The foundation specializes in MR-guided ultrasound. “The type of ultrasound that people are familiar with is for diagnosis, but there is a field of therapeutic ultrasound that includes ultrasound-guided and MRguided ultrasound. Some indications are better treated with MR-guided, and some are adequately treated with ultrasoundguided,” he said.
Another huge area for image-guided therapy is in the cardiovascular realm. A common procedure that uses imaging is the implantation of stents, small expandable tubes used to open blocked blood vessels, said Haemmerich. “For that, you need some kind of imaging to tell you where you are and where you want to go. That’s how you place the stents and then confirm that they are at the location you want them to be.”
Besides cancer and cardiovascular treatment, image-guided therapies are becoming more prevalent in orthopedic surgeries, such as minimally invasive knee replacements. The technology not only can provide the operating physician with a preoperative view of the affected joint but may also allow the operating physician to make adjustments during procedures so that joints can be aligned more precisely.
While it may not be an obvious connection, research into methods of drug delivery is also tapping imaging technology. When cancer patients receive chemotherapy today, drugs flood the entire body and the patients experience various side effects. “You’re kind of hoping that enough goes into the tumor,” Haemmerich said. “There’s currently a lot of research going on in terms of getting chemotherapy specifically into the tumor, and also getting radiation more concentrated in the region where the tumor is located. The idea is to get more into the tumor and to get less everywhere else in the body to reduce the side effects.”
Multiple hospitals are beginning clinical testing on image-guided liver and kidney surgeries, and Galloway said Vanderbilt hopes to do the first glaucoma treatment using image-guided therapy next spring.
“So the work goes forward,” he said. “We can never get enough NIH funding to have the people in place to work on this, but it’s going forward.”
AUTHOR
Leslie Mertz (LMERTZ@nasw.org) is a freelance science and medical writer and author as well as an educator.