Mobile Health: Revolutionizing Healthcare Through Transdisciplinary Research
By Santosh Kumar, Wendy Nilsen, Misha Pavel, and Mani Srivastava
NOTE: This is an overview of the entire article, which appeared in the January 2013 issue of Computer magazine.
Click here to read the entire article.
This article provides an overview and some specific examples of possibilities and shortcomings of the hardware and software underpinnings of mHealth, along with safety, efficacy, and privacy issues which must be addressed. The authors point out the need for collaboration between technical and medical personnel in this field.
Mobile health (mHealth) seeks to improve individuals’ health and well-being by continuously monitoring their status, rapidly diagnosing medical conditions, recognizing behaviors, and delivering just-in-time interventions, all in the user’s natural mobile environment. This approach offers tremendous benefits as the need for (and cost of) chronic care grows worldwide.
High-quality, user-friendly wireless consumer devices, such as mobile phones, have emerged that accompany users most of the time. Sensors in, or connected with, these devices can provide data to continuously assess a person’s health and risk factors. mHealth can build on mobile technologies, but much effort is needed in the fields of science and engineering to make it viable.
Figure 1 provides an overview of the mHealth process, from data collection by sensors to resulting intervention measures based on inferences drawn from that data.
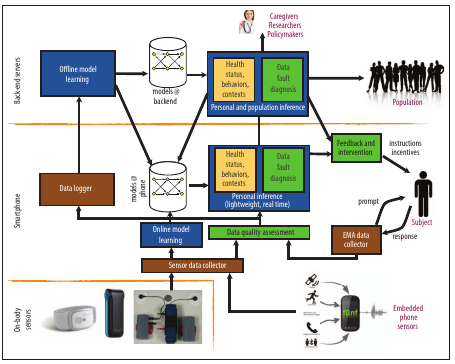
Figure 1. An overview of mobile health systems. Sensors at the lowest layer collect raw data that is processed to make inferences about individuals. These inferences can then be used to inform the design or delivery of just-in-time interventions and to make health inferences at the population level to inform health research, practice, delivery, and policy formulation.
At the sensor level, existing sensors often are not clinically relevant or do not provide sufficiently specific data. Sensors need to meet size and cost constraints and operate continuously in a way that does not burden the person to which they are attached. The article discusses biomedical, bioelectric, and imaging sensors in this regard, including examples which are making their way from research to practice.
But acquiring the data from sensors is not sufficient – the mHealth platform must be able to make significant and reliable inferences from this data. The authors review existing computing capabilities in mobile devices and point out the need for a “sensing stack” analogous to the existing networking stacks in these devices, to help transform the data.
Further, mHealth requires analytic functionality to derive actionable information from sensor data. Various conditions can compromise the quality of collected data; means are needed to recognize and correct for inaccurate, decreased quality data. Inference from the data needs to be based on reliable computational models – models that do not yet exist./p>
mHealth platforms should lead to appropriate intervention. The authors draw an analogy here to closing the loop in classical control systems. They discuss the concerns and potentials associated with intervention.
Finally, the authors present the design considerations associated with patient safety, the efficacy of the mHealth platform, privacy and security concerns, and the associated regulatory environment (in the US).
ABOUT THE AUTHORS
Santosh Kumar (santosh.kumar@memphis.edu) is an associate professor in the Department of Computer Science at the University of Memphis. His mHealth research interests include scalable physiological sensing, reliable inference of human health and behaviors, and realization of just-in-time interventions. He received a PhD in computer science and engineering from the Ohio State University. Kumar is a senior member of IEEE.
Wendy Nilsen (nilsenwj@od.nih.gov) is a health scientist administrator at the US National Institutes of Health Office of Behavioral and Social Sciences Research. Her scientific focus is on human behavior and behavior change, including utilizing mobile technology to better understand and improve health, adherence, the mechanisms of behavior change, and behavioral interventions in complex patients in primary care. Nilsen’s current mHealth efforts include addressing methodology and barriers to the utilization of mobile technology in research, serving on numerous federal mHealth initiatives, and leading the mHealth training institutes.
Misha Pavel (mpavel@nsf.gov) is a professor in the Department of Biomedical Engineering, with a joint appointment in the Department of Medical Informatics and Clinical Epidemiology, at the Oregon Health and Science University. He currently oversees the Smart Health and Well-being program at the US National Science Foundation. Pavel received a PhD in experimental psychology from New York University and an MS in electrical engineering from Stanford University. He is a senior member of IEEE.
Mani Srivastava (mbs@ucla.edu) is a professor in the Department of Electrical Engineering and is affiliated with the Department of Computer Science at the University of California, Los Angeles. His research interests include embedded wireless systems, power-aware systems, wireless networks, and pervasive sensing. Srivastava received a PhD in electrical engineering from UC Berkeley. He is an IEEE Fellow.






