Cancer Therapy through Nanomedicine
The National Cancer Institute’s plan to defeat cancer through engineered design.
By George W. Hinkal, Dorothy Farrell, Sara S. Hook, Nicholas J. Panaro, Krzysztof Ptak, and Piotr Grodzinski
Great strides have been made through biomedical research to alleviate the disease burden of many of the scourges of humanity. At the turn of the 20th century, infectious diseases were largely responsible for limiting the life expectancies in the United States to fewer than 50 years. Since then, groundbreaking discoveries in vaccines and antibiotics have decreased the deaths due to infectious disease in the developed world by nearly 100-fold [1]. By effectively removing this mortality factor from the equation, people began to live much longer. As a result, chronic diseases associated with the cumulative effects of life became more and more prominent.
Most prevalent among these are cardiovascular disease and cancer. Cardiovascular disease-related deaths have decreased upward of 50% since 1950 [1], [2], [3]. Meanwhile, although great strides have been made in the understanding of the science of cancer, cancer mortality has surprisingly remained recalcitrant to the point that it is now the top killer of persons younger than 85 years [4].
Cancer treatment has not changed much over the decades, where a regimen of surgery, radiation, and/or chemotherapy continue to be the therapeutic option, each with its own limitations. In surgical resection, it is often difficult to identify the boundaries of a tumor and/or the location of growing cancer before it spreads to other tissues. Chemotherapeutic treatments themselves are toxic to the body’s cells, albeit more toxic to the growing tumor, making systemic delivery wrought with secondary morbidities.
We at the National Cancer Institute’s Office of Cancer Nanotechnology Research (NCI,OCNR) believe that nanotechnology will provide the platforms from which a revolution in cancer therapy is possible (Figure 1). In this review, we will highlight some of the promising work, particularly those involving engineered devices and particles, emerging from our Alliance for Nanotechnology in Cancer (Alliance) that address the shortcomings in today’s cancer diagnosis and treatment regimen. The Alliance is composed of many of the nation’s leaders in the field of nanomedical research and is a model of success at the National Institutes of Health (NIH), where it has had among the highest and most impactful scientific output per grant dollar spent since its inception [5].
Collage of nanomedical particles and devices developed by Alliance members.
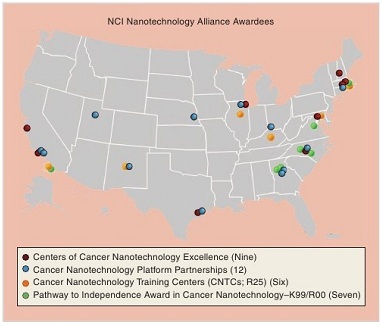
These groups comprise a nationwide network of research and training institutions that are driving this groundbreaking work (Figure 2). Major developments range between enhanced early diagnostics, novel therapeutic avenues, and improved monitoring and surveillance. By building novel devices on a nanoscale, researchers are taking advantage of recent cell and molecular biology discoveries and uniting them with cutting- edge materials science in a unifying, cross-disciplinary effort to transform cancer detection, diagnosis, treatment, and surveillance.
Map of the second phase of the Alliance for Nanotechnology in Cancer-funded centers and groups.
Improving Early Detection and Surveillance
By catching a cancer early in its development, survival outcomes are dramatically improved. Currently, screening is only available for a handful of cancers, and the efficacy of these methods has been questioned. A parallel concept is posttreatment cancer surveillance, where a clinician acquires cellular information during and after a patient’s treatment to determine the effectiveness of the given therapy, and again the patient would be screened for rare markers of disease. For both surveillance and screening, to detect a rare cancer cell that may initiate a tumor and/or circulating biomarkers, technologies need to be developed that reach several orders of magnitude of sensitivity greater than current practices. To this end, Alliance researchers have been developing devices and particles to detect cancer cells and biomarkers at unprecedentedly dilute levels.
At present, the gold standard diagnostic technique for detecting low levels of proteins is the enzyme-linked immunosorbent assay (ELISA). However, this method often limits which proteins can be analyzed and, after a protocol of several hours, provides a lower detection limit of approximately 10 pM. To circumvent this limitation, Dr. Shan Wang’s group at the Stanford CCNE has developed a method that is based on quantum principles of magnetism for detection [6]. This achieved resolution down to 50 aM that is linear over at least six logs of concentration. Remarkably, this procedure can be completed in just 15 min.
Another nanotechnology-based platform for monitoring cancer progression has come from work using gold nanoparticle (AuNP) probes for prostate-specific antigen (PSA) levels from the Northwestern University CCNE led by the research group of Dr. Chad Mirkin. Using current screening techniques, the limit of PSA detection is approximately 0.1 ng/mL; serum levels of patients who receive radical prostatectomy typically fall below this threshold, including both patients who remain disease free and those who relapse with deadly consequences. The Mirkin group designed a detection platform that uses an antibody sandwich technique which incorporates AuNPs and nucleic acids to facilitate detection and reading of analytes [7]. The Mirkin group could reproducibly detect PSA levels almost three orders of magnitude more sensitive than the current methods. This technology enables the delineation of cured patients from those with gradually increasing PSA levels, indicative of relapse, nearly one year sooner than current ELISA assays permit.
Cancer diagnosis is typically performed on tissue samples that have been surgically removed, but such biopsies only provide a snapshot of a tumor’s physiology. Often, by the time test results are produced, they may no longer be relevant. Hence, there is a goal to create a diagnostic platform that could continually monitor patients longitudinally to track how they are responding to treatment. Toward this goal, Dr. Michael Cima and his colleagues from MIT Harvard CCNE have developed an implantable device with the potential to measure biomarker concentrations as indicators of the local tumor environment [8].
Treating the Disease: Novel Cancer Imaging and Therapies
In many solid tumor cases, the most effective treatment remains surgical resection. However, today’s surgeons must rely on visual and tactile recognition of tumor locations and boundaries to determine what tissue to remove. Therefore, in many cases, too little or too much tissue is cut out leading to tumor regrowth or unnecessary secondary morbidities. Alliance researchers are developing novel nanoparticle based contrast agents to improve the existing imaging modalities such as MRI, and one group has developed a novel twist on a current imaging platform and is making headway toward its commercialization.
Clinical trials are expected to begin soon on a new type of CT scanner developed by Dr. Otto Zhou at the University of North Carolina (UNC) CCNE that uses carbon nanotubes (CNTs) as an X-ray source. This should reduce the imaging time and radiation dose while improving image resolution by reducing motion-induced blur. It has been validated as a promising tumor imaging technology, using breast phantom models, able to detect dense masses of just a few millimeters [9].
Glioblastoma multiforme (GBM) is the most common brain lesion, which is characterized by its aggressive growth and >95% mortality by five years postdiagnosis. Currently, the best treatment involves a combination of surgery, radiotherapy, and chemotherapy. Collectively, this standard regimen grants a median survival of 14.6 months and carries a significant risk of permanent secondary injury and profound neurological impairment [10]. To address this disease, the group led by Dr. Julia Ljubimova at the Cedars- Sinai Medical Center CNPP has been engineering a complex nanoplatform to pass through the BBB, target GBM, and deliver therapeutic agents. Using these methods, tumors were efficiently and specifically targeted and their growth dramatically retarded. Excitingly, this platform has recently been translated into another disease model and has proven similarly effective in treating breast cancer [11].
The laboratory of Dr. Peixuan Guo at the University of Cincinnati CNPP is engineering an entirely new class of cancer therapy platforms based on the RNA skeleton of the bacteriophage phi29’s DNA-packaging nanomotor. Some of the advantages of using RNA as a foundation of nanoparticle engineering are their capacity for in vivo self-assembly, their defined structure and stoichiometry, multivalency, and nonimmunogenicity. One of the successes in this field by the Guo laboratory has been to overcome the notorious sensitivity of RNA to RNase digestion. This should increase the clinical utility of recent results, where pRNA-based constructs were used to deliver silencing RNA sequences to cancer cells resulting in cell death [12].
Where Do We Go From Here?
The first phase of the NCI’s Alliance for Nanotechnology in Cancer, 2005-2010 promoted a convergence of specialists in oncology, materials science, biomedical research, and engineering to work together toward developing transformative nanotechnology for cancer medicine. The program was a remarkable success, producing more than 1,300 publications (with an average impact factor of 7.4), more than 250 patent disclosures and applications, dozens of spin-off companies, and several clinical trials [5].
The Alliance, in its second phase (2010-2015), is funding another batch of enthusiastic investigators. Central themes of this second phase are increased interinstitutional collaboration and leveraging funding toward greater clinical development with a goal of each CCNE sending at least one product into clinical studies by the end of the phase. Through this collective multiplatform expertise, collaboration, and ingenuity, we expect the contributions made by the Alliance toward fighting cancer to lead the way in breakthrough technology toward alleviating the burdens of cancer. We invite the reader to gain further insight and to follow the progress of the Alliance at our Web site at http://nano.cancer.gov/.
Acknowledgements
This project has been funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract N01- CO-12400. The content of this publication neither reflects the views or policies of the Department of Health and Human Services nor does it mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
About the Authors
George W. Hinkal (george.hinkal@nih.gov) received his Ph.D. degree in biomedical sciences from Baylor College of Medicine. In his postdoctoral work at the Centre Leon Berard, he developed transgenic mouse models of cancer metastasis. He is a fellow of the American Association for the Advancement of Science (AAAS) and Technology Policy and project manager for NCI’s OCNR (NIH, Bethesda, Maryland).
Dorothy Farrell (dorothy.farrell@nih.gov) received her doctorate in physics from Carnegie Mellon University, where her thesis project focused on the synthesis and characterization of self-assembled arrays of magnetic nanoparticles. She then spent two years at University College London, where she worked on the preparation of nanoparticle-antibody conjugates for use in cancer therapy. She returned to the United States to work at the Naval Research Laboratory before joining the NCI’s OCNR in 2008.
Sara S. Hook (sara.hook@nih.gov) holds a Ph.D. degree in pharmacology from the Duke University Program in Cellular and Molecular Biology. She looks after projects that use nanotechnology to enhance the understanding of cancer biology and use nanotechnologies for the delivery of genetic therapies. She participates in NCI-wide activities in research development for specific cancer types. Prior to joining the OCNR, she completed her postdoctoral work at Fred Hutchinson Cancer Research Center and at the University of Virginia.
Nicholas J. Panaro (panaron@mail.nih.gov) is currently a senior scientist at the Nanotechnology Characterization Laboratory, Advanced Technology Program, SAIC-Frederick Inc., Maryland.
Krzysztof Ptak (krzysztof.ptak@nih.gov) earned his Ph.D. degree in neuroscience from Paul Cezanne University in Marseilles, France, and Jagiellonian University in Krakow, Poland. He acts as a liaison between the program office and the bioinformatics community. He also coordinates communication between the program office and grantees. He has held research positions at Northwestern University and at the National Institute of Neurological Disorders and Stroke, NIH. His focus was on the neurobiology of respiration and specifically to the pathology of sudden infant death syndrome.
Click here to read the entire article, which appeared in the June 2011 issue of the IEEE Nanotechnology magazine.
- NCCDHP-CDC, “Achievements in public health, 1900-1999: Decline in deaths from heart disease and stroke-United States, 1900-1999,” Morbidity Mortality Weekly Rep., vol. 48, no. 30, pp. 649–656, 1999.
- K. D. Kochanek, S. L. Murphy, R. N. Anderson, and C. Scott, “Deaths: Final data for 2002,” Nat. Vital Statist. Rep.: From the Centers Dis. Contr. Prev., Nat. Center Health Statist., Nat. Vital Statist. Syst., vol. 53, pp. 1-115, Oct. 2004.
- N. L. Keenan and K. M. Shaw, “Coronary heart disease and stroke deaths-United States, 2006,” Morbitity Mortality Weekly Rep., vol. 60, no. 1, pp. 62-66, 2011.
- A. Jemal, R. Siegel, J. Xu, and E. Ward, “Cancer statistics, 2010,” CA Cancer J. Clin., vol. 60, no. 5, pp. 277-300, July 2010.
- K. Ptak, D. Farrell, N. J. Panaro, P. Grodzinski, and A. D. Barker, “The NCI Alliance for Nanotechnology in Cancer: Achievement and path forward,” Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol., vol. 2, no. 5, pp. 450-460, June 2010.
- R. S. Gaster, D. A. Hall, C. H. Nielsen, S. J. Osterfeld, H. Yu, K. E. Mach, R. J. Wilson, B. Murmann, J. C. Liao, S. S. Gambhir, and S. X. Wang, “Matrix-insensitive protein assays push the limits of biosensors in medicine,” Nat. Med., vol. 15, pp. 1327-1332, Nov. 2009.
- C. S. Thaxton, R. Elghanian, A. D. Thomas, S. I. Stoeva, J.-S. Lee, N. D. Smith, A. J. Schaeffer, H. Klocker, W. Horninger, G. Bartsch, and C. A. Mirkin, “Nanoparticle-based bio-barcode assay redefines ‘undetectable’ PSA and biochemical recurrence after radical prostatectomy,” Proc. Nat. Acad. Sci. USA, vol. 106, pp. 18437-18442, Nov. 2009.
- K. D. Daniel, G. Y. Kim, C. C. Vassiliou, F. Jalali-Yazdi, R. Langer, and M. J. Cima, “Multi-reservoir device for detecting a soluble cancer biomarker,” Lab on a Chip, vol. 7, pp. 1288-1293, Oct. 2007.
- X. Qian, R. Rajaram, X. Calderon-Colon, G. Yang, T. Phan, D. S. Lalush, J. Lu, and O. Zhou, “Design and characterization of a spatially distributed multibeam field emission X-ray source for stationary digital breast tomosynthesis,” Med. Phys., vol. 36, no. 10, pp. 4389-4399, 2009.
- S. A. Grossman, X. Ye, S. Piantadosi, S. Desideri, L. B. Nabors, M. Rosenfeld, and J. Fisher, “Survival of patients with newly diagnosed glioblastoma treated with radiation and temozolomide in research studies in the United States,” Clin. Cancer Res.: Official J. Amer. Assoc. Cancer Res., vol. 16, pp. 2443-2449, Apr. 2010.
- S. Inoue, H. Ding, J. Portilla-arias, J. Hu, B. Konda, M. Fujita, A. Espinoza, S. Suhane, M. Riley, M. Gates, R. Patil, M. L. Penichet, A. V. Ljubimov, K. L. Black, E. Holler, and J. Y. Ljubimova, “Polymalic acid-based nanobiopolymer provides efficient systemic breast cancer treatment by inhibiting both HER2/neu receptor synthesis and activity,” Cancer Res., vol. 71, no. 4, pp. 1454-1464, 2011.
- P. Tarapore, Y. Shu, P. Guo, and S.-M. Ho, “Application of phi29 motor pRNA for targeted therapeutic delivery of siRNA silencing metallothionein-IIA and survivin in ovarian cancers,” Mol. Ther.: J. Amer. Soc. Gene Ther., vol. 19, no. 2, pp. 386-394, Feb. 2011.