
New Probes Replace Surgeons’ Sense of Touch
New Probes Replace Surgeons’ Sense of Touch
As surgeons shift from open surgery to minimally invasive surgery, researchers look to new tools to help restore a surgeon’s sense of touch. A study at Vanderbilt University is developing a special purpose wireless capsule equipped with a pressure sensor that fits through the small ports that surgeons use for what is called “keyhole” surgery.
During open surgery, doctors rely on the ability to examine tissue through palpation to identify the hidden edges of tumors and locate hidden blood vessels and other anatomical structures. This process is not possible in minimally invasive surgery, technically known as laparoscopy, where surgeons use tiny, specialized instruments and miniature cameras that fit through small incisions.
Pietro Valdestri, a biomechatronics engineer at Vanderbilt University, and his research team showed IEEE Spectrum the wireless probe that a surgeon can manipulate in the body with a laparoscopic tool. Here’s how it works: The capsule’s pressure-sensing tip is used to gently indent the tissue. The magnetic field sensor and accelerometer track the depth of the indentation, along with its position relative to a stationary magnet nearby. Each point of contact transmits information about the stiffness of the tissue at that point. Using an algorithm to fill in any unexplored area, the computer creates a 3-D color-coded map that displays the tumors. Valdastri’s team has been testing their probe on a pig’s liver and on a chunk of synthetic tissue that contains tumor-like lumps.
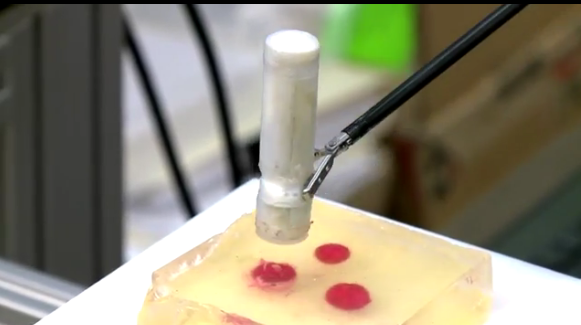
Capsule being demonstrated over simulated tissue. (from Vanderbilt University video)
Another group of researchers based at King’s College London and led by robotics expert Kaspar Althoefer, has devised an alternative to Valdestri’s probe. Althoefer’s probe consists of three surface-profile sensors equally spaced around a spherical indenter. As the probe glides over a tissue surface, the sphere, which floats on a pocket of air, indents the tissue, and a pair of optical fibers measures the indentation.
According to Robert Howe, a professor of engineering at Harvard University who developed some of the first remote palpation technologies, “If you ask surgeons, they’ll tell you that they need touch feedback, but then they go and perform a vast range of minimally invasive procedures without it.” Touch feedback is in the nice-to-have, mot the got-to-have category,” says Howe.
Researchers integrating palpation technologies into surgical robots are also still sorting out how to display the many layers of information to the robot’s operator. That has been a challenge for biomedical engineer Tim Salcudean at the University of British Columbia, in Vancouver. Using a technique dubbed vibro-elastography, he is generating 3-D elasticity maps by exciting tissue with vibration and measuring the waves produced using an ultrasound elastography probe. The probe is held by a surgical robot, which tracks its position.
“The new generation of surgeons are not doing a lot of open surgery, so they’re not used to palpation,” says Salcudean. With more than two million minimally invasive procedures being done in the U.S. alone, computer generated tissue maps may be the best way for surgeons to “feel” a tumor.






