Multifaceted Biomaterials Extend to Multiple Uses
By Leslie Mertz
NOTE: This is an overview of the entire article, which appeared in the July/August 2013 issue of IEEE Pulse magazine.
Click here to read the entire article.
Research is underway to uncover novel ways of making a wide range of medical devices biocompatible and to increase the level of biocompatibility of devices that are already biocompatible.
One of these research groups is led by Buddy Ratner, Ph.D., professor of bioengineering and chemical engineering, and the Michael L. and Myrna Darland Endowed Chair in Technology Commercialization at the University of Washington (UW), as well as director of University of Washington Engineered Biomaterials (UWEB), the university’s engineered biomaterials program. Ratner’s research team found a new way to make old material more biocompatible by adding engineered pores of a particular size and pattern to the material. They didn’t get the classic foreign body response where the body walls off the materials by surrounding them with a tough collagen sheath (scar tissue).
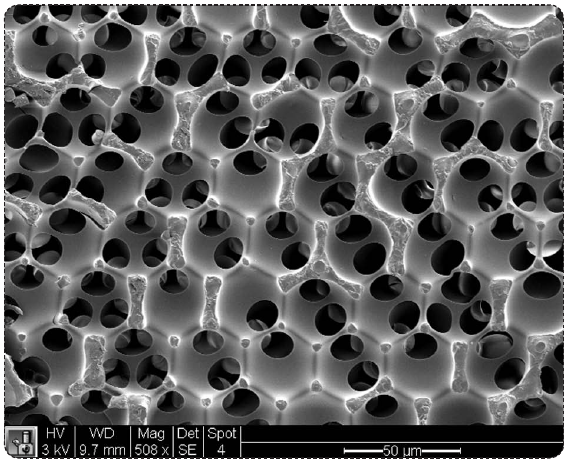
Ratner became interested in how the body would respond to a material that contained uniform, interconnected pores. He gave one of his doctoral students, Andrew Marshall, the task of generating such material. Marshall began using a process called sphere templating where microspheres, all of the same size, are packed down and surrounded with a monomer solution, then extracted away. Results of tests done where the resulting porous structures were implanted showed an integrated, vascularized healing rather than collagen encapsulation.
A research group at Michigan Technological University (MTU) in Houghton is developing materials that have the capacity to change shape when subjected to a magnetic field. The magnetic field causes the implanted materials to vibrate in a way that prevents cells growing over the implanted device from forming scar tissue, a common problem that shortens the lifespan of a device.
Another research group at MTU is developing biocompatible materials, this time focusing on nitric oxide (NO). The idea is to release controlled amounts of NO around a healing wound to promote the healing process. Megan Frost, Ph.D., assistant professor of biomedical engineering at MTU, and her group are finding novel ways of utilizing this to eliminate associated health risks and also prolong the lifespan of implanted devices.
A research group at North Carolina State University (NCSU) headed by Michael Dickey, Ph.D. an assistant professor of chemical and biomolecular engineering , was working to develop an new type of memory device that would be flexible . In conjunction with a group led by Orlin Velev, Ph.D., INVISTA Professor of Chemical and Biomolecular Engineering at NCSU, they serendipitously found that the memristor (memory resistor) they were able to create was biocompatible. This research is admittedly in the beginning stages, but is already being used to devise a replacement for standard electrocardiograph (EKG) probes.
According to Frost, “We may not ever reach a point where the artificial materials that we put in the body perfectly integrate to become completely part of the natural tissue, but I think what we can do is bridge a gap. We need materials that can continue to function and that will allow the body to actually rebuild itself.”






